50 year old female with left lower limb cellulitis with AKI,DM 2,HTN
- Get link
- X
- Other Apps
Introduction: This is an online E-log Entry Blog to discuss, understand and review the clinical scenarios and data analysis of patients so as to develop my clinical competency in comprehending clinical cases, and providing evidence-based inputs.
Note: The cases have been shared after taking consent from the patient/guardian. All names and other identifiers have been removed to secure and respect the privacy of the patient and the family.
Consent: An informed consent has been taken from the patient in the presence of the family attenders and other witnesses as well and the document has been conserved securely for future references.
CASE :
A 50 year old female came to GS OPD on 28-06-23 with complaints of
- swelling in left leg and foot since 1 week.
* The patient was apparently asymptomatic 1 week ago, then she developed swelling in the left leg which was insidious in onset.
It was associated with pain which was dragging type in nature, also associated with erythema. No aggravating or relieving factors.
H/o trauma - Pressure sore was manipulated with a blade.
No h/o Fever, nausea, vomitings, constipation.
No h/o similar complaints in the past.
The patient was on conservative treatment for her cellulitis i.e
1. Left limb elevation
2. Inj. Taxim 1gm IV/BD
3. Tab. PCM 650mg PO/BD
4. Tab. Chymoral forte PO/TID
** On 29-06-23, she was referred to GM i/v/o Elevated sugar levels, elevated Serum creatinine and elevated Serum urea.
FBS - 293mg/dl
S.Creatinine - 1.7
Urea - 53
---- The patient had complaints of
- Pain over the left lower limb
- Decreased appetite since 1 day
- Constipation since 1 year (passes stools once in every 3-4 days)
- Tingling and numbness of both the upper and lower limbs since 6 months.
No C/o polyuria, polyphagia, nocturia
No C/o fever, loose stools, vomitings, burning micturition
No C/o sob, palpitations, orthopnea, pnd, chest pain
The patient is a k/c/o DM-2 since 3 years and is on T.voglibose 0.2mg + T. Glimiperide 1mg + T. Metformin 500mg.
---- The patient was advised PLBS, HBA1C, USG - Abdomen and pelvis (i/v/o renal size, echo texture, rpd changes), CUE, ECG, 2D ECHO.
GRBS 7 point monitoring and Syp. Lactulose 15ml PO/TID was also adviced.
---- PLBS - 180 mg/dl; HBA1C - 7.0%
---- GRBS monitoring - On 30-06-23
8am - 180 mg/dl
10am - 239 mg/dl
2pm - 165 mg/dl
7pm - 172 mg/dl
10pm - 173 mg/dl
2am - 145 mg/dl
8am - 126 mg/dl
---- CUE - Albumin - 3+; Sugars - Nil; Pus cells - 2-4cells; Epithelial cells - 4-6cells;
RBC - 24-26 cells
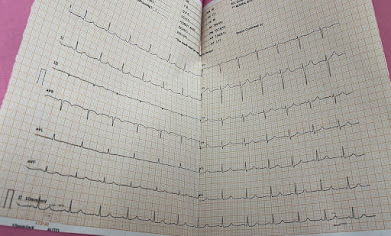
---- ECG - Poor R wave progression
** On 01-07-23, the patient was again referred to GM i/v/o vomitings and headache.
---- The patient had complaints of
- vomitings since last night, about 10 episodes with food as content, non projectile, non bilious, non blood stained
- Head ache and neck pain since yesterday
The patient has been shifted to General medicine for the stabilisation of the patient's general condition.
Past history :
- She is a k/c/o DM - 2 since 3 years, and is on Tab. Voglibose 0.2mg + Tab. Glimiperide 1mg + Tab. Metformin 500mg.
- Not a k/c/o HTN, Bronchial asthma, epilepsy, seizures, thyroid disorders.
Appetite - reduced; Mixed diet; Regular bowel and bladder movements; Reduced sleep (due to pain); No known allergies, No addictions.
Family history :
Insignificant
General examination :
Patient is C/C/C and well oriented to time, place and person.
No signs of pallor, icterus, cyanosis, clubbing, edema, lymphadenopathy.
Vitals - On 01-07-23
Afebrile on touch
BP - 180/100 mmhg
PR - 88bpm
RR - 18cpm
Spo2 - 96% at RA
Systemic examination :
CVS - S1, S2 heard, no murmurs
RS - BAE +, NVBS heard
CNS - NAD
PA - Soft, non tender, no organomegaly.
PROVISIONAL DIAGNOSIS :
Left lower limb cellulitis with AKI with Hypertensive crisis with Type 2 DM with Diabetic retinopathy.
?Nephritic syndrome ?Diabetic nephropathy ?Acute gastritis
Investigations :
CBP -
ON 28-06-23
ON 30-06-23
LFT -
ON 28-06-23
ON 29-06-23
RFT -
ON 28-06-23
ON 02-07-23
Blood Urea - 122 mg/dl**
Serum Creatinine - 6.0 mg/dl**
Sodium - 135 mEq/L**
Potassium - 5.3 mEq/L**
Chloride - 98 mEq/L
Calcium ionised - 1.08 mmol/L
ON 03-07-23
BT - 2MINS 30 SECS
CT - 5 MINS
PT - 14 SECS
INR - 1.0
APTT - 35 SECS
ESR ON 29-06-23 WAS 122*
CRP - ON 29-06-23 WAS POSITIVE 1.2MG/DL
BGT - AB +VE
Serology - Negative
CT done on 01-07-23
Review 2D ECHO done on 01-07-23
Review USG done on 03-07-23
Treatment :
01-07-23 - SOAP NOTES
--S : 10 episodes of vomitings with food as content, non projectile, non bile stained, non blood tinged. Also complains of headache and neck pain.
--O : Patient is C/C/C
Afebrile on touch; BP - 180/100mmhg; PR- 88/min; RR - 18cpm; Spo2 - 96% on RA
CVS - S1, S2 heard, no murmurs; CNS - NAD; RS - BAE+, NVBS; PA- Soft, non tender, no organomegaly.
--A : Left lower limb cellulitis with AKI with Hypertensive crisis with Type 2 DM
? Nephritic syndrome ? Acute gastritis
--P : 1. NBM until further orders.
2. IV fluids - NS, RL @ 100ml/hr.
3. Left lower limb elevation.
4. Tab. Nicardia 10mg PO/QID
5. Inj. Pan 80mg in NS over 4 hours.
6. Inj. Zofer 4mg IV TID
7. Syp. Lactulose 15ml PO/TID
8. Tab. Limcee PO/OD
10. Strict GRBS 7 point monitoring.
11. Strict input/output charting.
12 Monitor vitals and inform SOS.
02-07-23 - SOAP NOTES
--S : Vomitings subsided but patient complaints of nausea and loss of appetite.
--O : Patient is C/C/C
Temp - 98.4F ; BP - 170/100mmhg ( on labetolol - 1.5ml/hr) ; PR- 84/min; RR - 16cpm; Spo2 - 96% on RA; GRBS - 129mg/dl; I/O - 1800/200ml
CVS - S1, S2 heard, no murmurs; CNS - NAD; RS - BAE+, NVBS; PA- Soft, non tender, no organomegaly.
--A : Left lower limb cellulitis with AKI with Hypertensive crisis with Type 2 DM
? Nephrotic syndrome ? Acute gastritis
--P : 1. Allow fluids.
2. IV fluids - NS, RL - 30ml + hourly urine output
3. Left lower limb elevation.
4. Inj. Labetolol @4mg/hr (increase/decrease according to MAP)
5. Inj. Pan 40mg IV OD
6. Inj. Zofer 4mg IV TID
7. Tab. Nicardia 10mg PO/QID
8. Syp. Lactulose 15ml PO/TID
9. Tab. Limcee PO/OD
10. Strict GRBS 7 point monitoring.
11. Strict input/output charting.
12. Monitor vitals and inform SOS.
03-07-23 - SOAP NOTES
--S : Patient complaints of abdominal pain Weakness since morning
Giddiness since morning
Urine output has reduced.
Vomitings have subsided.
--O : Patient is C/C/C
Temp - 98.2F ;
BP - 170/90mmhg ;
PR- 82/min; RR - 22cpm; Spo2 - 94% on RA. Input/output - 1650/90ml.
CVS - S1, S2 heard, no murmurs;
CNS - NAD;
RS - BAE+, B/L basal crepts present in Infra axillary area, mammary area, Infra scapular area.
PA- Soft, non tender, no organomegaly.
--A : Left lower limb cellulitis with Stage 5 CKD with Hypertensive crisis with Type 2 DM with Diabetic retinopathy
? Nephritic syndrome
?Acute gastritis
--P : 1. Liquid to soft diet
2. IV fluids - NS @ 30ml/hr + hourly urine output
3. Left lower limb elevation.
4. Tab. Labetalol 100mg PO/BD
5. Inj. Pan 40mg IV BD
6. Inj. Zofer 4mg IV TID
7. Tab. Nicardia 10mg PO/QID
8. Syp. Lactulose 15ml PO/TID
9. Tab. Arkamine 0.1mg PO/OD
10. Strict GRBS 7 point monitoring,
Inj. HAI S/C TID as per advice.
11. Strict input/output charting
12.Monitor vitals and inform SOS
- Get link
- X
- Other Apps